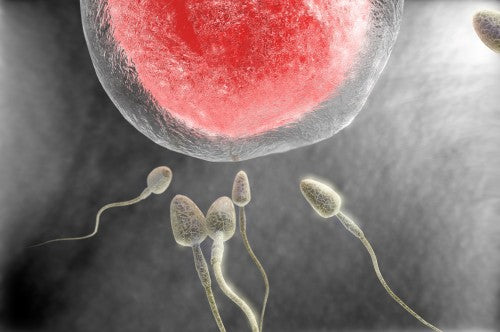
Does Abstinence Help to Improve Sperm Count?
Abstinence won't improve your chances of getting pregnant. Studies have shown that men with normal sperm count and motility can go a bit over a week without ejaculation, and sperm health doesn't suffer.
If you have sperm health issues, you should only abstain for a day for the best quality sperm.
Additionally, if you abstain for too long, you could cause harm to your sperm. The motility and morphology of your sperm will deteriorate if you abstain for over a week. As you might suspect, this is extremely damaging when it comes to conception.
Thus, the studies state that men should ejaculate between three and four times a week to ensure proper motile, healthy sperm.
A Study About Abstinence and the Ability to Conceive
Eliahu Levitas, a fertility specialist in the IVF unit of Israel's Soroka University Medical Center, conducted a study to examine sperm samples from approximately 6,000 men. All the samples were from men who had abstained from intercourse for up to two weeks. Most of the men in the study had normal sperm counts. About one-third of the men had low sperm count.
Researchers also discovered that sperm motility decreased through a day of abstinence for men with low sperm counts. Additionally, other changes were occurring concerning shape, a telltale sign that sperm health was rapidly declining.
However, it is essential to note that men with normal sperm counts demonstrated little change in motility following abstinence. They didn't show signs of sperm health decline until much later.
What Does This Mean for Me?
The studies show abstinence is mainly irrelevant for couples with normal fertility.
They also show that men with low sperm counts can benefit from abstaining for a day or two. This ensures there is more healthy sperm available.
Abstinence should not extend beyond the two-day mark as there is no benefit.
Of course, increased frequency of intercourse is ideal for couples trying to conceive, and you shouldn't be waiting for ovulation to occur have sex. Having sex every 2 to 3 days throughout the cycle ensures sperm will be waiting to fertilize the egg.
However, this doesn't mean that intercourse should be excessive because you risk depleting your sperm storage. Instead, you should focus on keeping your system flushed to ensure that sperm are fresh.
Sperm that hangs around for longer than necessary run the risk of damage. The sperm becomes less likely to fertilize the egg. Following ejaculation, it takes one to two days for sperm to recoup their numbers.
Another study shows that 14 days of daily ejaculation leads to lower semen volume, sperm count and hindered motility. All issues that make getting pregnant more difficult.
Ways to Improve Your Sperm Count and Quality
Since abstinence isn't the answer, what can you do to help improve your sperm quality?
There are plenty of things that will improve your sperm count, motility, and morphology. Chances are, without knowing it, you are doing things that harm your sperm. If you stop doing them, your sperm health will improve.
What about the things you could be doing but aren't? You can add many things to your day-to-day life that will improve your sperm. Are you willing to do what it takes?
Improved sperm health means you have better odds of getting pregnant.
Resources
Pellestor F, Girardet A, Andreo B. Effect of long abstinence periods on human sperm quality. Int J Fertil Menopausal Stud. 1994 Sep-Oct;39(5):278-82. PubMed PMID: 7820161.
Levitas E, Lunenfeld E, Weiss N, Friger M, Har-Vardi I, Koifman A, Potashnik G. Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples. Fertil Steril. 2005 Jun;83(6):1680-6. PubMed PMID: 15950636.
Welliver C, Benson AD, Frederick L, et al. Analysis of semen parameters during 2 weeks of daily ejaculation: a first in humans study. Translational Andrology and Urology. 2016;5(5):749-755. doi:10.21037/tau.2016.08.20.
Tags:
About Sperm
Quick links
Search
Contact Us
Shipping Information
Helpful Info
Terms of Service
Privacy Policy
Do not sell my personal information
Contact us
About us
BabyHopes.com is a family owned and operated business, opened in January 2001. We have been serving the trying to conceive community for over 20 years.

