Understanding Low Sperm Count and Tips for Supporting Male Fertility
For men, fertility is a multifaceted issue influenced by lifestyle, environment, age, and other health factors. Low sperm count is one factor that can impact a couple's journey to conceive, but it’s important to remember that having a low sperm count does not necessarily mean that conception is impossible. With the right information, support, and a few lifestyle changes, men can take proactive steps toward supporting reproductive health.
This article will explain what low sperm count means, explore potential lifestyle factors, and offer practical tips to help support overall sperm health.
What is Low Sperm Count?
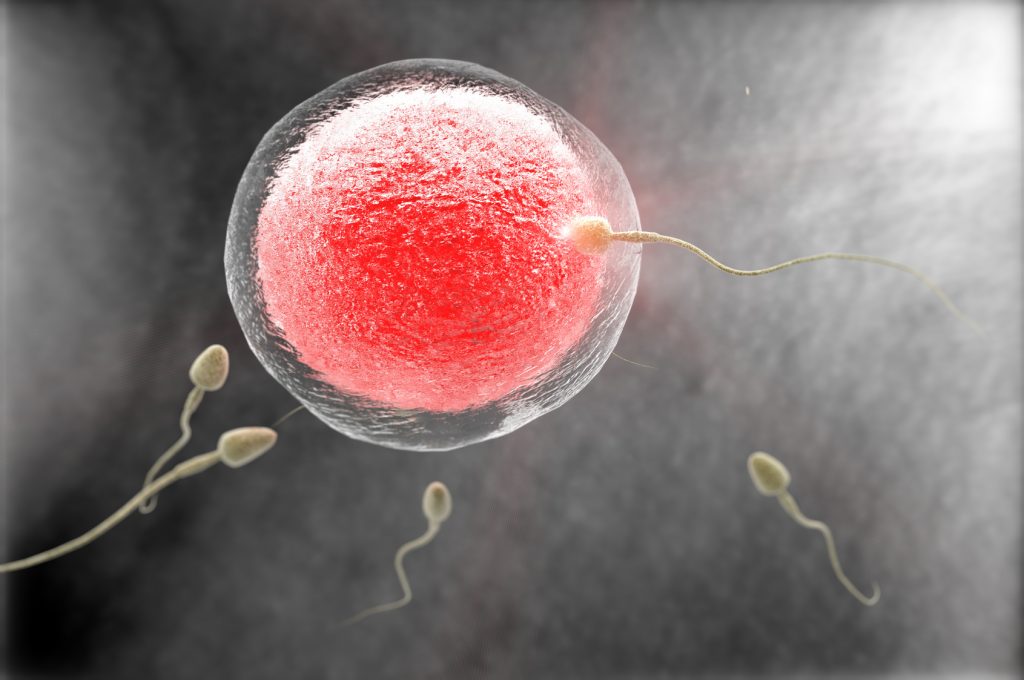
Low sperm count, also known as oligospermia, means that the amount of sperm present in the semen is below a certain level. According to the World Health Organization (WHO), a sperm concentration below 15 million sperm per milliliter (15 million/ml) of semen is classified as low. While it only takes one sperm to fertilize an egg, a healthy sperm count can improve the likelihood of successful fertilization.
Low sperm count can affect the chances of conception, and it’s essential for men to know that fertility is influenced by a variety of factors, not just sperm count alone. Many men with low sperm counts still achieve natural conception, while others benefit from fertility treatments or lifestyle adjustments to support reproductive health.
Factors That Can Influence Sperm Health
There are several lifestyle and environmental factors that may impact sperm count and overall sperm quality. Here’s an overview of some common influences:
-
Chemical Exposure
Frequent exposure to industrial chemicals, pesticides, and heavy metals has been linked to changes in sperm health. Men who work with these substances may want to consider protective measures or consult a healthcare provider about ways to minimize exposure. -
Heat Exposure
Sperm thrive in an environment that’s slightly cooler than body temperature. Prolonged exposure to heat, such as wearing tight clothing, sitting for extended periods, or frequenting saunas and hot tubs, can temporarily affect sperm production. -
Radiation Exposure
X-rays and other sources of radiation can affect sperm quality, particularly without protective measures. If X-rays are required, using a protective apron can help shield reproductive organs from radiation exposure. -
Age
Although men can produce sperm throughout their lives, research suggests that sperm quality and quantity may naturally decline with age. Men over 35 who are trying to conceive may consider talking to a healthcare provider about how age-related changes could affect fertility.
Lifestyle Tips for Supporting Sperm Health
Men can take proactive steps to support sperm health through lifestyle and dietary changes. These approaches are not guaranteed solutions, but they are associated with positive impacts on reproductive health.
1. Regular Exercise
Staying active supports cardiovascular health, hormone balance, and general wellness, which may all contribute to reproductive health. Moderate, consistent exercise can help manage weight and improve energy levels, though it’s important to avoid overexertion, as excessive exercise can potentially impact hormone levels.
2. Avoid Smoking
Research shows that smoking may negatively affect sperm count and quality. Tobacco smoke introduces toxins and heavy metals into the body, which can impact both sperm motility and morphology. Additionally, secondhand smoke exposure has been linked to fertility issues in women, which means quitting can benefit both partners.
3. Review Medications with a Healthcare Provider
Certain medications, such as anabolic steroids, some antibiotics, blood pressure medications, and antidepressants, may impact fertility. Men concerned about the impact of medications on reproductive health can speak with a healthcare provider or pharmacist to discuss potential alternatives or adjustments.
4. Consider Nutritional Supplements
Some nutrients are associated with supporting reproductive health, including vitamin C, zinc, folic acid, and Coenzyme Q10. Here’s a brief overview of their roles:
- Vitamin C: Known for its antioxidant properties, vitamin C may help support sperm motility and structure.
- Zinc: This mineral, especially when combined with folic acid, has been associated with supporting sperm production.
- Folic Acid: Folic acid may support sperm count and is often recommended as part of a balanced diet for reproductive health.
- Coenzyme Q10 (CoQ10): This antioxidant has been associated with supporting sperm motility and overall quality in some studies.
Before starting any supplement, consult a healthcare provider to ensure it’s appropriate for your health needs.
5. Manage Stress
Long-term stress can affect hormone levels, which in turn may impact sperm production. Practicing stress management techniques, such as meditation, breathing exercises, or mindfulness, can support overall wellness and may indirectly benefit reproductive health. Simple daily practices, like taking breaks and engaging in hobbies, can help reduce stress levels.

Healthy Eating for Male Reproductive Health
Diet plays a vital role in supporting reproductive health, and incorporating certain nutrients through food sources can be a practical approach. Here are some nutrients and food sources often associated with supporting male fertility:
- Vitamin C: Bell peppers, strawberries, dark leafy greens, broccoli, and citrus fruits
- Zinc: Beef, shrimp, pumpkin seeds, and spinach
- Omega-3 Fatty Acids: Salmon, walnuts, flax seeds, and dark green vegetables
- Selenium: Tuna, shrimp, turkey, and Brazil nuts
- Folic Acid: Leafy greens, broccoli, beans, and lentils
Prioritizing a nutrient-dense diet filled with whole foods may support overall wellness, including reproductive health. Whenever possible, consider choosing organic and sustainably sourced foods.
Supplements for Supporting Sperm Health
Adding a fertility supplement to a balanced diet may provide an additional source of nutrients associated with reproductive health. Supplements that include ingredients like folic acid, zinc, vitamin C, and CoQ10 can support overall sperm health. However, it’s essential to choose high-quality products and consult with a healthcare provider before starting any new supplements.
When to Consider a Fertility Assessment
If you and your partner have been trying to conceive for a while without success, a fertility assessment may provide insights into potential factors impacting conception. Many healthcare providers recommend fertility assessments after one year of trying to conceive, or after six months if either partner is over 35.
Home Sperm Testing
For those seeking preliminary insights, at-home sperm count tests are available. These tests can give a general idea of sperm count, but they do not assess other aspects of sperm health, such as motility or morphology. If results indicate low sperm count or other concerns, consulting a fertility specialist is the next step for a comprehensive evaluation.
The Importance of Professional Guidance
Male fertility is influenced by a range of factors, from genetics to lifestyle choices. Speaking with a healthcare provider can offer valuable insights and recommendations tailored to your unique health profile. Fertility specialists can help identify potential concerns and recommend strategies or treatments to support reproductive health.
Summing It All Up
While low sperm count can impact fertility, many factors can support reproductive health, from lifestyle adjustments to nutrient-dense diets. Here’s a summary of helpful steps:
- Maintain a healthy lifestyle, including regular exercise and balanced nutrition.
- Avoid smoking, excessive alcohol consumption, and limit exposure to environmental toxins.
- Consider supplements associated with sperm health, but consult with a healthcare provider.
- Seek professional advice if trying to conceive for more than a year, or six months if over age 35.
The journey to parenthood is unique for each couple, and staying informed and supported can make a meaningful difference along the way.
Tags:
About Sperm
Quick links
Search
Contact Us
Shipping Information
Helpful Info
Terms of Service
Privacy Policy
Do not sell my personal information
Contact us
About us
BabyHopes.com is a family owned and operated business, opened in January 2001. We have been serving the trying to conceive community for over 20 years.
